Can You Have a Kidney Stone Without Pain
 Agonizing, intolerable, miserable, excruciating, stabbed with a knife, worse than childbirth.
Agonizing, intolerable, miserable, excruciating, stabbed with a knife, worse than childbirth.
As a urologist specializing in the handling of patients with kidney stones I take learned a new dictionary exclusive to stone formers describing bouts of renal colic.
Pain, the hallmark symptom of stone illness, accounts for over one million emergency room visits by such patients in the United States each year.
Over the past several decades considerable progress has been made gaining insight into the physiology of renal colic and optimizing methods to care for it. Nevertheless, despite improved scientific explanations we equally clinicians still lack a perfect understanding of why information technology occurs.
Hurting FROM Rock PASSAGE
Patients have been suffering from renal colic secondary to rock disease for over ii thousand years. As a matter of fact, information technology is remarkable how little has changed in its clinical presentation over this time period. In 400 B.C. Hippocrates referred to information technology equally first illness of the kidneys. He was one of the initial observers to cover the association between urinary obstacle and pain, writing:
An acute pain is felt in the kidney, the loins, the flank and the testis of the affected side; the patient passes urine frequently; gradually the urine is suppressed. With the urine, sand is passed; every bit the sand passes along the urethra, it causes severe pain which is relieved when it is expelled; then the aforementioned sufferings brainstorm again.
Nosotros take since come to appreciate the circuitous physiologic basis for this relationship at a much deeper level.
How Hurting Begins
 The first step in this process is acute obstruction, most commonly from a stone. But in stone formers masses of crystals tin can create obstacle, every bit can claret clots if bleeding is specially brisk.
The first step in this process is acute obstruction, most commonly from a stone. But in stone formers masses of crystals tin can create obstacle, every bit can claret clots if bleeding is specially brisk.
Urine from the kidney can no longer pass to the bladder and as a issue builds upward and stretches the proximal – closest to the kidney – ureter and renal collecting organization. This stretch activates nociceptive nervus fibers – fibers which sense injury – within an entire neuronal network located submucosally in the renal pelvis, calyces, capsule and ureter.
Figure 1 (left) – Example of obstructing proximal ureteral stone with dilation and stretch of the collecting organisation above the level of obstruction.
These fibers then transmit afferent signals to the T11 – L1 spinal string which the trunk interprets equally pain at the corresponding level of neuronal activation . As the stone migrates from the kidney down the ureter and towards the bladder, pain unremarkably shifts downwardly as well. It is usually sensed as high equally the upper flank when the stone is lodged in the proximal ureter and as low equally the labia/testicle when down near the uretero-vesical junction at the entry to the bladder.
Patients passing stones may experience other symptoms in addition to pain. Many of the nerves involved in the process of obstruction are intimately linked to innervation of adjacent organs, for case the gastrointestinal tract. Cross activation of these associated nerve fibers has been proposed equally an explanation for the nausea and vomiting which so often occurs in the setting of an astute episode of renal colic.
In rare instances patients may even take alternative symptoms without any pain at all. In some cases, especially when the stone is at the uretero-vesical junction, urinary symptoms predominate and the only observable symptoms are urinary frequency, urgency and discomfort while voiding. These symptoms mimic urinary infection and often upshot in temporary mis-treatment with antibiotics until the correct diagnosis is fabricated.
What Happens Later
Increasing renal pelvis pressure level from persistent obstruction causes a release of prostaglandin E2. This chemical mediator of injury response produces a perfect storm.
Information technology causes ureteral hyperperistalsis (increased intensity of the waves of coordinated ureteral contractions which normally drive urine down to the float) and eventually fifty-fifty ureteral spasm. It also leads to dilation of the afferent arterioles – those tiny resistance vessels which command the flow of claret into the capillaries of the kidneys.
The arteriolar dilation increases blood flow to the kidney and promotes a temporary diuresis only as ureteral smooth muscle hyperperistalsis and ultimately spasm tighten the ureter around the rock and worsen obstruction. Spasm leads to lactic acid build upwards, as occurs when any muscle is over-exercised, and sets off an inflammatory cascade that itself tin worsen pain.
With time, claret flow to the afflicted kidney falls, even though the arterioles which let blood into the renal capillaries remain dilated. Information technology falls because the efferent arterioles, which let blood out of the capillaries where filtration occurs, begin to tuck and raise filtration by the renal glomerulae . The increased filtration maintains and tin even raise pressures.
Figure ii – Diagram of claret menstruation to the nephron. Blood enters through the afferent arteriole and is so filtered within the glomerulus, producing urine in the procedure. Blood exits through the efferent arteriole. Both the afferent and efferent arteriole are able to dilate and constrict in club to regulate pressure and ultimately filtration via urine production.
In many ways, this complex system is analogous to the soaker hoses many people use to water their lawns. The afferent arterioles are the faucet the hose is continued to and the efferent arterioles are the opening at the end of the hose which can be closed or left open into a sprinkler.
Filtration is the many tiny flows of h2o all along the hose which go along the grass growing.
When working accordingly, the faucet and the finish are both open up and water (urine) is produced at a slow, constant rate (Figure 4 – left). With an obstructing stone the faucet – so to speak – is opened more and the stop clamped more than then more fluid – water – is filtered out along the length of the hose at loftier pressure (Figure 4 – right). In the kidney this filtration is into the nephrons and raises pressure. When the clamp is tightened, the total amount of flow through the hose can autumn merely every bit the corporeality of h2o filtered out along the hose rises.
Figure 4 – Soaker Hose Analogy to Renal Blood Flow and Filtration. On the left, there is piddling pressure in the system and h2o (urine) seeps out slowly from along its length. On the right, the inflow is much higher than the outflow and water (urine) shoots out from along the hose at exceedingly high pressure level.

Three Phases of Pain in more than Detail
The Physiology
No word regarding ureteral obstruction would be complete without the work of Eastward. Darracott Vaughan , who characterized the physiology of urinary obstruction in the 1970'southward.
Assuming two functional kidneys, the physiologic furnishings of acute unilat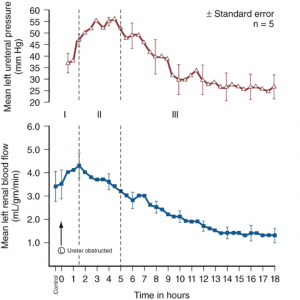 eral ureteral obstruction tin be marked by iii distinct phases .
eral ureteral obstruction tin be marked by iii distinct phases .
In phase one, the furnishings of the inflammatory cascade described higher up cause a progressive rise in renal blood period and renal pelvis and ureteral force per unit area. This phase lasts for approximately ane to i and a one-half hours. This is the portion where the afferent arteriole – the faucet – is maximally opened.
Phase two is marked by efferent arteriolar vasoconstriction which causes a subtract in overall renal claret catamenia but an increment in ureteral pressure for up to five hours. The faucet is opened and the end clamp is tightened.
Phase iii is marked past a farther decrease in renal blood flow to the afflicted kidney and ultimately decreased ureteral force per unit area. The end clamp is progressively tightened and then blood flow to the kidney is reduced enough that filtration and urine production begin to fall, and pressure level with it.
Measurements of ureteral pressure (cerise) and renal blood period (blue) after onset of acute unilateral ureteral obstacle. (Courtesy Campbell-Walsh Urology, Tenth Edition, Elsevier Inc.)
The autumn in blood flow is non injurious during an acute assail, but over fourth dimension it can be. This means that relief of an obstructing rock is an important matter. Commonly stones pass of themselves. But stone attacks need medical attention because if the rock continues to obstruct it must be removed.
The Symptoms
Information technology is easy to conjecture how these three distinct phases correlate clinically to the symptoms experienced during an acute episode of colic.
The onset of pain classically correlates to stage one and the inciting obstructive result. It is at this point that the patient commonly seeks intendance in the emergency room or physician'south office.
The pain classically persists at a astringent level for several hours (phase two) but ultimately subsides, at least partially (phase iii).
In many instances hurting comes in waves, potentially a sign of intermittent obstruction activating the in a higher place pathway each time urinary menstruation is obstructed. This occurs through a combination of the stone moving and the tensions of the ureter with increases or decreases of muscle spasm.
THE Puzzler – Pain Without Obstacle
Opinions of Urologists in General
Though the physiologic basis of pain in the setting of obstruction is clear, information technology does not provide an explanation for one of the most commonly encountered conundrums in rock affliction – the symptomatic non -obstructing stone. These tin be actual free stones that have non passed, stones attached to plaque , or actual plugs in the kidney tubules that are massed together enough to bear witness upward on a CT scan as 'stones' though actually tissue calcifications.
There is mayhap equally much variation in clinical opinion in such instances every bit whatsoever other clinical scenario in the field.
If one were to inquire a grouping of urologists whether they believed that pocket-size nonobstructing stones could cause renal colic, opinions would range from accented certainty to complete dismissal of the concept altogether.
What Happens to Patients
As a result, at that place is no standard of care regarding how to optimally manage such patients. In all cases information technology is first imperative to dominion out other potential sources of hurting; however, such workups often end with the aforementioned result – a patient with bothersome flank pain and evidence of ane or more nonobstructing stones on imaging.
Lacking a physiologic caption to explain their symptoms, patients with pain and not obstructing stones are oft sent for detailed workups, secondary and tertiary consultations and referral to pain specialists and even psychiatrists. Notwithstanding, in an age where flexible ureteroscopy can be performed quite safely and on an outpatient footing one must wonder whether such patients are existence treated appropriately.
A Specific Instance
As an example, I recently met a patient who had been referred from several hours away seeking a fourth stance regarding her chronic flank pain. For months she had suffered from a severe anguish in her left flank that had limited her ability to work and live her normal life.
She had attributed the pain to a vii mm lower pole nonobstructing renal stone on that side which was discovered on a CT scan during her initial presentation to an outside emergency room (Effigy 3). However, none of the physicians she had seen agreed with her self diagnosis.
scan during her initial presentation to an outside emergency room (Effigy 3). However, none of the physicians she had seen agreed with her self diagnosis.
Figure iii – CT image of left lower pole nonobstructing stone (red pointer). There is no evidence of obstruction or inflammation around the kidney.
In the ER she was given narcotic pain medication and sent abode to follow-up with a urologist.
The kickoff urologist she saw told her that while the stone was visible, its location within the kidney meant that it could non possibly be causing her hurting. He refilled her prescription for pain medication and sent her to meet a hurting specialist.
The hurting specialist tried physical therapy for what he thought may be a musculoskeletal source but ultimately this did not prove effective and she was given more than pain medication.
She later sought care from a second urologist who as well told her that the stone could not possibly exist causing her pain in the absence of obstruction. This time however she was defendant of having an agenda and seeking care specifically to become pain medication. Similar visits to a variety of emergency rooms elicited more CT scans as well as accusations of seeking pain medications. Each CT result was the same though, all demonstrating a vii mm non obstructing left lower pole stone.
On one example a treating practitioner even admonished her, saying that nonobstructing stones don't cause pain and he should know since he also had been diagnosed with such stones incidentally on a CT browse.
Ultimately she fabricated her way to the clinic for consultation at which bespeak she was offered a ureteroscopy and stone removal. The procedure went well and she was discharged with a stent for one calendar week. She was terminal seen back 5 weeks after the procedure and reported complete resolution of her hurting. She was no longer taking any pain medication whatsoever and at that place was no evidence of any rock or hydronephrosis on follow-upwardly imaging.
What is Known to Date
Such patients are frequently encountered. Despite a lack of physiologic explanation as to why these non-obstructing stones may cause pain, at that place is emerging evidence that they do and therefore that removal tin can cure it.
In 2006 Taub et al . described outcomes of 20 such patients who had chronic flank pain as well equally radiographically evident calcifications inside their papillae without obvious collecting system stones. Ureteroscopy with laser papillotomy to unroof and remove all axiomatic stone was performed on twenty 7 kidneys. Pain improvement was seen in 85% of cases with a durable improvement for greater than one year in nearly sixty% of cases.
This study was and then repeated on a multi-institutional level with 65 patients undergoing similar procedures over a ten year period. Overall there were 176 procedures performed in this cohort with patients reporting less pain later on the procedure 85% of the time. The mean duration of response was 26 months with 60% of patients having sustainable improvements in their pain levels for over i yr.
Finally, this clinical scenario is seen ordinarily enough that information technology garnered its own nickname at Massachusetts General Infirmary where it has been described equally "small rock syndrome". In a retrospective review of patients treated there with ureteroscopic removal of modest nonobstructing stones (<4mm) for reasons related to chronic hurting, 11/13 patients reported being pain free after the procedure with the other 2 noting a partial response.
What I recall
Nosotros withal exercise not completely understand the physiologic caption for pain in these patients. However, much like Hippocrates over 2 thousand years agone, clinical observation often precedes scientific understanding. In this regard it is unfair to dismiss the notion that small not obstructing stones tin arm-twist legitimate renal colic.
Physiologic breakthroughs in the agreement of pain signaling and inflammation are currently happening at a rapid charge per unit and it is probable that in time we may be able to improve decipher which non-obstructing stones are truly responsible for symptoms. Notwithstanding, until so, such scenarios will continue to be a commonly encountered clinical complexity for urologists.
For the time being I would still abet consideration of culling causes of pain in such situations including urinary infection, obstruction and malignancy. A conscientious history is critical to rule out not-urologic sources such as pathology within the musculoskeletal, pulmonary, gynecologic and gastrointestinal systems. Some other important chemical element of the history is whether the patient has previously passed a stone and if the current symptoms are similar to that experience.
In one case other explanations have been ruled out, offer stone removal is entirely reasonable. This not only has the potential to improve hurting but may likewise decrease the risk of futurity stone growth or spontaneous passage at a later date. In such instances, I prefer flexible ureteroscopy with stone removal to shock moving ridge lithotripsy. Commencement, ureteroscopy maximizes the likelihood that all stones can be identified and removed which is specially important in the event that pain persists after the procedure. 2nd, with ureteroscopy 1 tin inspect the inside of the kidney in high definition which has the potential to offering information not readily available on 10-rays and CT scans such as embedded stones, tissue calcifications, and other pathology ( Figure 4 ).
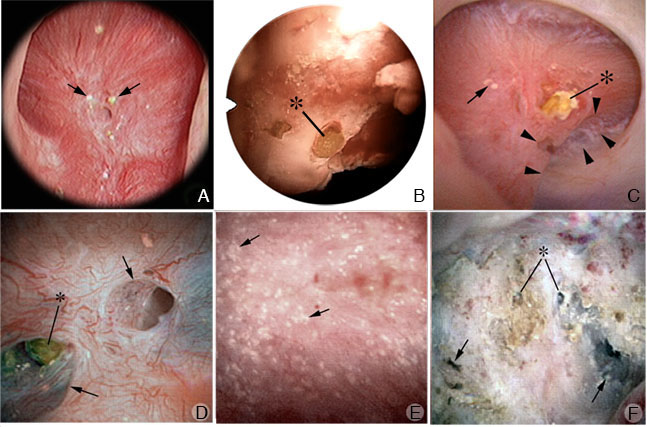
Figure iv – Loftier definition images obtained during renal endoscopy demonstrating tubular plugging (stones embedded in the kidney) (Courtesy: AE Evan, IMCD and BD plugs: Do they take a role in stone germination).
Finally, it is critical to establish realistic expectations before surgery in regards to hurting control. Our agreement of this concept is in development and the published literature suggesting a treatment response is express to relatively few patients. However, as scientific discipline and history have shown united states, merely because we don't fully sympathise the connection doesn't mean it doesn't exist.
More You lot Might Like
What Kidney Stones Are
Types of Kidney Stones
Practice Nosotros Need to Analyse All Those Stones?
How Kidney Stones Class
When Crystals Plug The Kidneys
Medullary Sponge Kidneys
catchingsspladebeforn.blogspot.com
Source: https://kidneystones.uchicago.edu/why-do-kidney-stones-cause-pain/
0 Response to "Can You Have a Kidney Stone Without Pain"
Post a Comment